Cholesterol
& Statins: Part II
by Yusuf M. Saleeby, MD
to be published in American Fitness magazine (Mar/April 2013 issue)
In the last
issue (Cholesteron & Statins : Part I, American
Fitness Jan/Feb 2013), the discussion centered on cholesterol, that
necessary but often maligned molecule. The
previous article made one realize that this steroid compound is a double edged
sword as it relates to health concerns.
While essential for the life of human cells, high serum levels of total
cholesterol and in particular elevated non-HDL-cholesterol, designated bad
cholesterol, end up being harmful to our cardiovascular system.
Plenteous
research, time and money have been devoted to the study of this low density
lipoprotein substance that carries cholesterol (LDL-C) out of the liver to
cells. It was discovered that too much
would ‘’clog up’’ arteries back in the 1970s.
This was the driving force for aggressive development of medications to
combat the formation and lower the level of LDL-C in circulation.1
As previously
mentioned in Part I, dietary restriction of cholesterol is of limited
value. When we limit our oral intake of
dietary cholesterol, our body produces cholesterol in the liver to compensate
for a predetermined genetic set point.
Thus a cholesterol restrictive diet alone is usually not enough to
reduce markedly elevated levels of the ‘’bad cholesterol.’’ 2 Dietary
restrictions alongside weight loss and exercise are a more effective approach. Lipid lowering medications like the class of
statin drugs have a more potent affect.
History:
Statins or
HMG-CoA reductase inhibitors are a class of drug that inhibits an enzyme which plays
a central role in manufacturing cholesterol in the liver. The term ‘’statin’’ is derived by the last
few letters of some of the original drugs developed, lovostatin and simvastatin
being examples. Historically, the
Japanese biochemist Dr. Akira Endo isolated the first statin drug (mevastatin),
but it showed toxicities and never made it to market. Not long afterwards in the early 1970’s
researchers from Merck pharmaceuticals following up on published research and
developed the first marketable statin (lovostatin) which was extracted similar
to Dr. Endo’s from the fungus (Aspergillus
terreus).1,3 Incidentally, there are naturally occurring statins,
namely those found in the oyster mushroom (Pleurotus
ostreatus) and the extracts from fermented red yeast rice fungi (Monascus purpureus).4 This
latter extract is used commercially as a natural alternative to reduce
cholesterol.
Merck capitalized
on the statin drugs Zocor® and Mevacor®, which earned the company over $1-Billion
each by 1995. Dr. Endo was also the
beneficiary of the 2006 Japan Prize and Lasker-DeBakey Clinical Research Award
in 2008 for his achievements in the field of lipid chemistry. Today there are a number of statins in the
marketplace, as both stand alone drugs and in combination with other lipid
lowering agents. Names the public would
recognize include Lipitor® (atorvastatin), Lescol® (fluvastatin), Mevacor® (lovastatin),
Pravachol® (pravastatin), Crestor® (rosuvastatin) and Zocor® (simvastatin). All are lab synthesized drugs except for
lovastatin and pravastatin which are derived directly from naturally occurring yeast
and bacterium.
Statin Drugs (HMG-coA reductase inhibitors)
Numerous
medical trials show the statins as having a major affect on lowering LDL-C, and
thus bringing the total cholesterol in serum down. Statins can, with varying degree raise HDL-C
levels. When compared to diet alone,
statins are proven more effective in lowering LDL-C. However, this is not accomplished without
some undesirable side effects. The drugs
mostly affect the liver hepatocytes and muscle cells. The toxicity of natural occurring statins in
mushrooms is unobtrusive, but some serious muscle damage can occur with
pharmaceuticals. One such incident
occurred when Baycol® (cerivastatin) came to market some years ago. It was so toxic that the Federal Drug
Administration (FDA) had to remove it from pharmacies in 2001.5
Recent
changes to the National Institute of Health (NIH) guidelines for testing
individuals now suggest that children between the ages of 9 to 11 have lipid
screening performed. Most statins are approved
for use in children 10-years and older, but use should be judicious. Statins are classified as Category X in
pregnancy which means they are contraindicated in expectant women because of high
risk of birth defects.6
Statin drugs
produce muscle pain in approximately 30-percent of individuals who take them. Other side effects include liver damage,
digestive problems, rash, cataracts, an increase in blood glucose and type-2
diabetes (T2DM) risk, and neurological conditions as a rise in amyotrophic
lateral sclerosis (ALS) incidence. Those
that are at higher risks are females, those taking other cholesterol
medications, people with small body frames and with underlying kidney or liver
disease and/or diabetes. Being over the
age of 65-years also increases risk for untoward effects for statin users. There are reports of a fifty-percent increase
in risk of developing age-related cataracts with those using statin drugs
compared with non-users.5,6,7
To combat
detrimental side effects, sometimes a prescriber will switching from one statin
to another, or reduce the dose, or change the dosing schedule to every other
day. If a person is taking a statin they
should avoid grapefruit and grapefruit juice as this can potentiate the drug’s harmful
effects. The cardiac rhythm drug
amiodarone (Cardarone®) has an interaction with simvastatin. Lopid® another lipid lowering agents concomitant
use with statins is ill advised. Some
HIV drugs (protease inhibitors) interact with lovastatin in a negative way. There are even interactions with antibiotics
and antifungal drugs. The
immunosuppressant drug cyclosporine (Sandimmune®) can increase risk for
rhabdomyolysis (muscle breakdown) as well.5,7 With
statin use monitoring of liver function tests (transaminases) and muscle
biomarkers creatine kinase (CPK) and aldolase are indicated routinely along
with monitoring the effects of the drug to meet goal (serum LDL-C and ApoB
levels). Yet other measures to reduce
untoward effects of statin drugs have been to add coenzyme Q10, correct Vitamin
D and thyroid deficiencies, or switch to a non-statin regimen. There is a theoretical risk that lowering
cholesterol drastically can affect production and levels of beneficial steroid
hormones. More study in this area is
needed to confirm or dispel fears.
Since the
mapping of the human genome, genetic tests have been developed to help predict
coronary risk and the effectiveness of statin therapy. The blood test analyzing the KIF6 genotype (offered
by Berkeley Heart Labs) may aid doctors in directing lipid therapy as
polymorphisms in this gene identify those at higher risk for coronary heart
disease. Once identified, those
individuals can reduce their risk with statin therapy. The SLCO1B1 genotype test, help clinicians
predict who may be at greater risk for muscle damage while on lipid lowering therapy. Carriers of the SLCO1B1 gene are more likely
to have problems with statin induced myopathy then those who do not carry that
gene.8,9
With the drug
market eventually becoming saturated with statin medications and coming under
fire with a plethora of side effects, researchers began looking elsewhere. Focus was centered on manipulation of
beneficial lipoproteins, namely HDL-C.
It was reasonable to think that raising HDL-C would scavenge the bad
cholesterol away to be recycled and thus not be around to form foam cells. Research had already proven that reduction in
native LDL-C and foam cells, which lead to arterial plaque formation, would
lessen the risk for heart disease. A
genetic malady, albeit rare gave promise that developing pro-HDL-C drugs may be
a superior alternative to statin therapy.
Tangier Disease afflicts a very small number of people worldwide, but
with extremely low levels of HDL-C there is a tendency for more advanced
cardiovascular disease in younger victims.10-13 Initial trials of HDL-C raising drugs were a
disappointment to those proponents of raising HDL, but research continues in
this direction.14
In all
fairness to statin drugs, there have been reports of other benefits such as
improving endothelial function, reducing inflammatory C-Reactive Protein,
coronary plaque stability and reduction in thrombus formation (clots). Additionally, for reasons not quite clear
there was a reduction in cancer risk while study subjects were on statin drugs.15,16
According to
an October 2012 JAMA report on trends in lipids in the United States between
1988 and 2010, total cholesterol and LDL-C numbers experienced a
reduction. Unfortunately during the same
time frame triglycerides (TG) went up while HDL-C remained unchanged. This is all apparently the result of
aggressive statin use with Americans having dyslipidemia.17
Pharmaceutical Alternatives to Statin
Therapy
Ezetimibe a
drug known in the US market as Zetia® is an alternative for those who cannot
tolerate statin therapy. Ezetimibe can
lower cholesterol by interrupting intestinal re-absorption of cholesterol. However, studies have reported continued use
can thicken the arterial walls. So it is
recommended as a drug of last resort by some.
Ezetimibe is also used in conjunction with statins in some dual agent
drugs such as Vytorin®. Dual therapy is
a means of using two agents at lower individual doses to achieve a particular
lipid level goal and limit side effects.18,19
Fibric Acid
derivatives such as gemfibrozil (Lopid®) and fenofibrate (TriCor®) are other
alternatives to statin therapy. While
not as effective in lowering LDL-C as stains, they do raise HDL-C and lower Triglycerides
(TG). Fibric Acid drugs are known to
improving insulin resistance as an added benefit. However, in combination with statins they can
increase risk for liver and muscle injury.20,21
Vitamin B3
(nicotinic acid) in high doses is commonly used to raise HDL-C. This naturally occurring substance while relatively
safe in high doses does come with the undesirable side effect of flushing. Flushing can be thwarted by a delayed release
delivery system (Niaspan®) by prescription and by premedication with low dose
aspirin.22
Questran®
and WelChol® are in a class of drug called bile acid resins. Bile acid resins are used to lower LDL-C and
total Cholesterol by sequestration and expulsion in feces. They are effective and are another
pharmaceutical alternative with limited systemic effects used in statin-intolerant
patients.22
Cholesteryl
ester transfer protein (CETP) inhibitors came on the scene recently. They were touted as the new wonder drug for
cholesterol management, or so it was thought.
This class of medication is used to raise HDL-C.12,13 However, initial attempts by Roche
pharmaceuticals were halted in phase III trials due to failure of the agent (torcetrapid)
to perform safely.14 Nonetheless,
the Academy for the Advancement of HDL Science is optimistic about future
developments and new drugs in the pipeline.15
Natural Alternatives to Statin
Therapy
Fish oil is
a clinically proven agent in lowering cholesterol and triglycerides. The omega-3 fatty acids docosahexaenoic acid
(DHA) and eicosapentaenoic acid (EPA) are well researched as being effective
for dyslipidemia. Krill oil is a newer arrival into the
forum; it has been peddled as being better than fish oil by proponents. Having a lower DHA and EPA content than fish
oil and costing 5 to 10-times as much, it may not be a preferred choice. Only a few high concentrated Krill or
Krill/Fish oil combinations give you the necessary concentrations of DHA/EPA to
lower lipids and provide cardiac risk reduction.23 Fish oil has the FDA nod of approval for
lowering cholesterol and triglycerides (TG) and even comes as the FDA approved
prescriptive Lovaza®. While Lovaza® is
rather expensive; those seeking pharmaceutical grade fish oil have many less
expensive choices that are equally effective and safe. Caution should be taken when using fish oil with
other blood thinning medications prior to elective surgery or with those with
seafood allergies.
Besides fish
oil there are several herbal and dietary supplements that can lower cholesterol
and heart disease risk. Garlic in some
studies reported a reduction of total cholesterol by a few points. Caution however, must be taken when taken in conjunction
with blood thinners such as Coumadin® as bleeding risks may increase.24 Oat bran and barley have been studied and demonstrate
that with regular ingestion a person can lower cholesterol and cardiac risk.25
The resin
Guggulipid derived from the mukul myrrh tree, illustrates a reduction of LDL-C
and total cholesterol in clinical studies performed in India. Demonstrating Guggulipid to be an important natural
lipid lowering agent will require more scientific examination. As mentioned earlier the extract of fermented
red yeast rice is a naturally occurring statin.
While showing lower risk of toxicity, there is a linear correlation with
lower effectiveness due to its reduced potency.
The product of the waxy coating of sugar cane and beet skins known as policosanol
was shown in several clinical trials to lower LDL-C when taken orally in
standard doses.24,26,27
Extracts of
fenugreek, artichoke, yarrow, and holy basil may also help lower cholesterol,
but again clinical trials will have to prove this to the medical community. The use of ginger, turmeric, and rosemary in
cholesterol lowering preparations are common as there may be some benefit. Consumption of dietary fiber, soy based foods,
and plant sterols (aka phytosterols, compounds similar to cholesterol) can
reduce LDL-C. Phytosterols interfere
with the re-absorption of cholesterol and can be found in commercial bread
spreads like Benecol®, Promise®, and Smart Balance®.26,27 With the advent of ‘’Medical Foods” there are
patented combination therapies, sanctioned by the FDA for prescriptive use,
that have shown promise in scientific studies.
Metagenic’s UltraMeal360® is an example of such a prescriptive medical
food.28 Another medical food
is Hypertensa® designed for those with metabolic syndrome by Physician
Therapeutics; and more of these safer alternatives are on the horizon.29
Whether you put
your chips on lowering LDL-C or raising HDL-C one important fact remains; both
courses of action will reduce cardiovascular risk, but when you add weight loss
and exercise then risk of heart disease really drops. According to Mayo Clinic reports, weight loss
of between 5 and 10 lbs can lower LDL-C levels.
For every six pounds of weight loss you can increase HDL-C by 1mg/dL in
serum levels. Physical activity, as in
sustained exercise, lasting 30 minutes or more at least five times a week can
yield a five-percent increase in HDL-C.
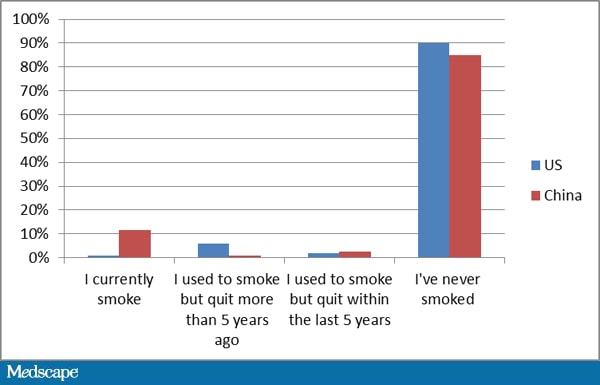
Smoke cessation is also a big player; quit smoking and you can increase
your HDL-C by ten-percent and in a year reduce your heart disease risk by
fifty-percent.26,27,30,31
Controlling
cholesterol is a complicated process for physicians and patients alike. Wrought with drug tolerance, unproven
alternatives, and cost issues, it is a daunting task to manage
dyslipidemia. Along with ever changing
practice guidelines for serum cholesterol levels offered up every couple of
years by national medical societies and institutions, therapeutic
recommendations will likely remain in flux for the unforeseeable future.
References:
1. Endo A., The discovery and
development of HMG-CoA reductase inhibitors, J. Lipid Res. 1992;33 (11): 1569–82.
2.
Ahmed SM,
Clasen ME, Donnelly JE. Management of dyslipidemia in adults. Am Fam Physician, 1998;1;57(9):2192-2204,
2207-8.
3. Simons, John. "The $10
billion pill", Fortune magazine, January 20, 2003.
4. Liu J, Zhang J, Shi Y, Grimsgaard S,
Alraek T, Fønnebø V, Chinese red yeast rice (Monascus purpureus) for primary hyperlipidemia: a meta-analysis of
randomized controlled trials". Chin
Med 2006;1: 4.
5. Golomb BA, Evans MA., Statin Adverse
Effects: A Review of the Literature and Evidence for a Mitochondrial Mechanism. Am J Cardiovasc Drugs 2008;8(6):
373–418.
6. Prescriber’s Letter, January 2012 (vol. 19, no. 1) and June 2012 (vol. 19, no. 6) section on
Statins and Dyslipidemia.
7. Statin Side Effects, Retrieved from http://www.mayoclinic.com/health/statin-side-effects/MY00205
(Accessed 12/3/2012)
8. SLCO1B1 Genotype testing, Retrieved
from http://www.bhlinc.com/clinicians/test-descriptions/SLCO1B1-Genotype-Test
(Accessed 12/3/2012)
9. KIF6 Genotype testing, Retrieved from
http://www.bhlinc.com/clinicians/test-descriptions/KIF6, (Accessed 12/3/2012)
10. Grover SA,
et al., Evaluating the incremental benefits of raising high-density lipoprotein
cholesterol levels during lipid therapy after adjustment for the reductions in
other blood lipid levels. Arch. Internal
Med. 2009;169:1775.
11. Singh IM,
et al., High-density lipoprotein as a therapeutic target: A systematic review. JAMA. 2007;298:786.
12. High
Cholesterol: Cholesterol-lowering medication, Retrieved from
http://www.webmd.com/cholesterol-management/guide/cholesterol-lowering-medication,
(Accessed 12/3/2012)
13. HDL Cholesterol: How to boost your
‘good’ cholesterol, Retrieved from
http://www.mayoclinic.com/health/hdl-cholesterol, (Accessed 12/3/2012)
14. "Roche provides update on Phase
III study of dalcetrapib." Roche press release, May 7, 2012.
15. Academy for the Advancement of HDL
Science, Retrieved from http://lipid.org (Accessed 12/3/2012)
16. Ridker PM,
Danielson E, Fonseca FAH et al., Rosuvastatin to prevent vascular events in men
and women with elevated C-reactive protein. NEJM 2008;359 (21): 2195–207.
17. Mitka M., Cholesterol drug
controversy continues. JAMA 2008;299 (19):
2266.
18. Carroll, MD., et al, Trends in Lipids
and Lipoproteins in US Adults, 1988-2010., JAMA,
2012;308(15):1545-1554.
19. Garcia-Calvo M, Lisnock J, Bull HG,
Hawes BE, Burnett DA, Braun MP, et al. The target of ezetimibe is Niemann-Pick
C1-Like 1 (NPC1L1). Proc Natl Acad
Sci, 2005;102(23):8132-7.
20. Jun M, Foote C, Lv J, et al., Effects
of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet 2010;375 (9729):
1875–1884.
21. Steiner G., Atherosclerosis in type 2
diabetes: a role for fibrate therapy?. Diab
Vasc Dis Res, 2007;4 (4): 368–74.
22. Alternative Treatments for High
Cholesterol, Retrieved from http://www.webmd.com/cholesterol-management/guide/high_cholesterol_alternative-therapies,
(Accessed 12/3/2012)
23. Krill Oil: A substitute for Fish oil?
Prescriber’s Letter August 2010, Retrieved from
http://prescribersletter.therapeuticresearch.com (Accessed 12/3/2012)
24. Cholesterol-lowering supplements:
Lower your numbers without prescription medication, Retrieved from
http://www.mayoclinic.com/health/cholesterol-lowering-supplements/CL00013
(Accessed 12/3/2012)
25. Jenkins, D.
[Oats bran and Barley on Cholesterol] American
Journal of Clinical Nutrition, 2005; vol 81:pp 380-87.
26. Alternative Cholesterol Treatments,
Retrieved from http://naturaldatabase.therapeuticresearch.com (Accessed
12/3/2012)
27. Alternative Cholesterol Treatments,
Retrieved from Cleveland Clinic Department of Nutrition and Cleveland Clinic
Heart Center web sites (Accessed 12/3/2012)
28. Metagenics
UltraMeal360®, Retrieved from
http://www.metagenics.com/products/health-conditions/hypercholesterolemia,
(Accessed 11/16/2012)
29. Hypertensa®
Package Insert, Retrieved from http://tmedpharma.com/docs/monographs-5-22/Hypertensa_Product_Monograph_for_website_5-22-08.pdf
(Accessed
11/16/2012)
30. Smith SC Jr, Benjamin EJ, Bonow RO,
et al., AHA/ACCF secondary prevention and risk reduction therapy for patients
with coronary and other atherosclerotic vascular disease: 2011 update: a
guideline from the American Heart Association and American College of
Cardiology Foundation endorsed by the World Heart Federation and the Preventive
Cardiovascular Nurses Association. J
Am Coll Cardiol. 2011;58(23):2432-2446.
31. Greenland P, Alpert JS, Beller GA, et
al., 2010 ACCF/AHA guideline for assessment of cardiovascular risk in
asymptomatic adults: a report of the American College of Cardiology
Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2010;122(25):e584-e636.
----
Yusuf (JP) Saleeby, MD is medical
director of WellnessOne and WellnessFirst which offer extensive and advanced
cardiovascular and stroke biomarker and genetic analysis, including lipid
subtypes, Lp(a), CRP, HDL2 and HDL3, LDL1-4,
ApoB, NT-proBNP, Lp-PLA2, and the 4q25, 9p21, ApoE, KIF6 and SLCO1B1-Genotype tests. He is a
regular contributor to American Fitness
and serves on the medical advisory board.
He can be reached for comment at ymsaleeby@gmail.com.


 This will take you to the new saleeby.net site
This will take you to the new saleeby.net site